Embark on a comprehensive journey through the pleural effusion nursing care plan, a roadmap for healthcare professionals to effectively manage this condition. Delve into the intricacies of assessment, interventions, monitoring, patient education, and documentation, empowering nurses to provide exceptional care.
This meticulously crafted guide unravels the complexities of pleural effusion, providing a thorough understanding of its signs, symptoms, diagnostic tests, and the crucial monitoring of vital signs and respiratory status. Discover evidence-based interventions to alleviate symptoms, prevent complications, and enhance patient outcomes.
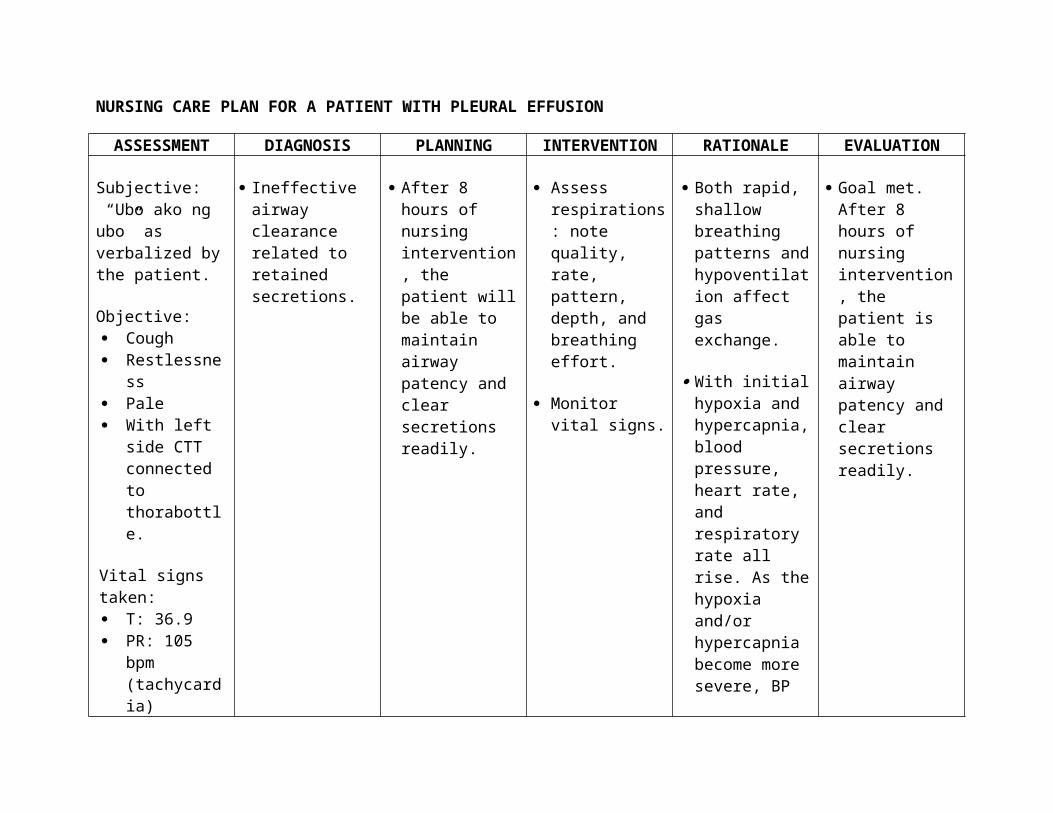
Assessment: Pleural Effusion Nursing Care Plan
Assessing pleural effusion involves recognizing its signs and symptoms, performing diagnostic tests, and monitoring the patient’s vital signs and respiratory status.
Signs and Symptoms
- Shortness of breath (dyspnea)
- Chest pain, often sharp and stabbing
- Cough, which may be dry or produce frothy sputum
- Fatigue and weakness
- Fever
Diagnostic Tests
- Chest X-ray:Shows the presence and extent of pleural effusion.
- Thoracentesis:A needle is inserted into the pleural space to withdraw fluid for analysis.
- Ultrasound:Uses sound waves to visualize the pleural space and assess fluid accumulation.
- CT scan:Provides detailed cross-sectional images of the chest, allowing for precise localization of the effusion.
Monitoring Vital Signs and Respiratory Status
Monitoring vital signs, including heart rate, respiratory rate, and oxygen saturation, is crucial to assess the patient’s overall condition and respiratory function. Changes in these parameters may indicate a worsening of the effusion or complications.
Interventions
Effective management of pleural effusion involves a multifaceted approach that addresses symptom relief, complication prevention, and improved patient outcomes. Interventions range from non-invasive measures to invasive procedures, tailored to the individual patient’s needs and underlying etiology.
Thoracentesis
Thoracentesis, also known as pleural tap, is a minimally invasive procedure that involves aspirating fluid from the pleural space. It serves both diagnostic and therapeutic purposes. Diagnostic thoracentesis helps identify the nature of the pleural effusion (e.g., transudate, exudate, or empyema) and determine its underlying cause.
Therapeutic thoracentesis relieves respiratory distress by removing excessive fluid, improving lung expansion, and facilitating oxygenation.
Chest Tube Insertion
Chest tube insertion, also known as tube thoracostomy, is a more invasive procedure involving the placement of a chest tube into the pleural space. It is indicated when thoracentesis is ineffective or when ongoing drainage is necessary. Chest tubes are used to evacuate fluid, air, or both from the pleural space, re-expand the lung, and prevent complications such as pneumothorax or empyema.
Monitoring and Evaluation
Monitoring the patient’s response to treatment is crucial in managing pleural effusion. Regular assessments of the patient’s symptoms, physical examination findings, and imaging studies are necessary to determine the effectiveness of the treatment and identify any potential complications.
Criteria for Discontinuing Thoracentesis or Chest Tube Drainage
- Resolution of dyspnea and chest pain
- Absence of pleural fluid on chest X-ray or ultrasound
- Stable vital signs
- No evidence of infection or complications
Potential Complications of Pleural Effusion and Management
- Empyema:Infection of the pleural space. Management includes antibiotics, drainage, and potential surgical intervention.
- Fibrothorax:Thickening and scarring of the pleural space. Management includes pleurodesis or surgical decortication.
- Trapped lung:Inability of the lung to re-expand after drainage. Management includes chest physiotherapy, bronchoscopy, or surgery.
Patient Education
Understanding how to manage your pleural effusion at home is crucial for your recovery and well-being. This section provides guidance on self-care, follow-up care, and recognizing signs of complications.
Self-Care Management
- Monitor your weight regularly to track fluid retention.
- Limit fluid intake as directed by your healthcare provider.
- Elevate your head and shoulders while resting or sleeping to improve fluid drainage.
- Avoid smoking and exposure to secondhand smoke, as they can worsen fluid buildup.
- Engage in light exercise or daily walks to promote fluid movement.
Follow-Up Care and Monitoring, Pleural effusion nursing care plan
Regular follow-up appointments are essential to monitor your condition and adjust treatment as needed. Your healthcare provider may order chest X-rays or other tests to assess fluid levels and check for complications.
Recognizing Complications
It’s important to be aware of signs and symptoms that may indicate complications, such as:
- Increased shortness of breath or difficulty breathing
- Chest pain or tightness
- Fever or chills
- Coughing up blood or purulent fluid
- Rapid heart rate or irregular heartbeat
If you experience any of these symptoms, seek immediate medical attention.
Documentation
Accurate and timely documentation is crucial in the care of patients with pleural effusion. It serves as a legal record, facilitates communication among healthcare professionals, and provides a basis for quality improvement initiatives.
Assessment
- Document the patient’s history, including symptoms, onset, and any potential risk factors.
- Record the results of the physical examination, including vital signs, respiratory assessment, and chest auscultation.
- Note any diagnostic tests performed, such as chest X-ray or thoracentesis.
Interventions
- Document all nursing interventions provided, including medication administration, oxygen therapy, and chest tube management.
- Record the patient’s response to interventions, including any changes in symptoms or vital signs.
- Document any complications or adverse events that occur.
Outcomes
- Document the patient’s progress towards expected outcomes, such as improved respiratory function or resolution of pleural effusion.
- Note any changes in the patient’s condition or any deviations from the expected trajectory.
- Record any patient education provided and the patient’s understanding of the information.
Key Questions Answered
What are the common signs and symptoms of pleural effusion?
Shortness of breath, chest pain, dry cough, fatigue, and decreased breath sounds.
How is pleural effusion diagnosed?
Through a physical exam, chest X-ray, ultrasound, and thoracentesis.
What is the purpose of thoracentesis?
To remove fluid from the pleural space and relieve pressure on the lungs.